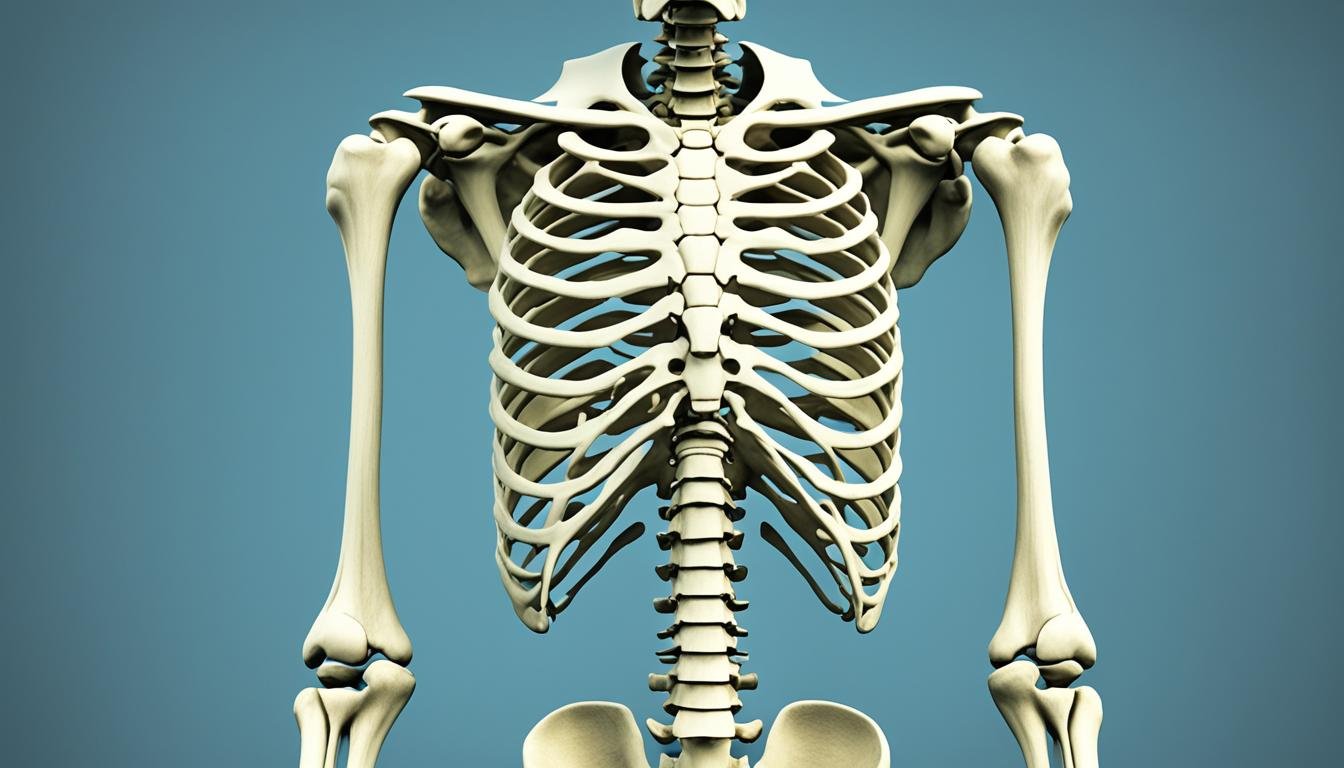
Osteoporosis is a bone disease that weakens your bones over time.1 As your bone mass decreases, it becomes easier to get fractures. Broken bones are a big risk for people with osteoporosis.
This disease is hard to notice because it doesn’t show early symptoms. You might not realize you have it until you break a bone.1 It’s common in older adults, notably after menopause for women.
Osteoporosis can affect anyone, regardless of their background. The chances of getting it rise as you age.1 Thus, it’s crucial to take care of your bone health throughout your life.
Key Takeaways
- Osteoporosis is a bone disease that leads to decreased bone density and increased fracture risk.
- Osteoporosis is often a “silent” disease, with no symptoms until a fracture occurs.
- Fractures associated with osteoporosis most commonly occur in the hip, spine, and wrist.
- Osteoporosis affects individuals of all races and ethnic groups, but certain factors like age, gender, and hormonal changes can increase the risk.
- Lifestyle factors such as physical activity, diet, and smoking can impact bone health and the development of osteoporosis.
What is Osteoporosis?
Osteoporosis is a bone disease that makes your bones weaker and more likely to break.1 It is often unnoticed because it shows no symptoms. You may only realize you have it after breaking a bone.1
Definition of Osteoporosis
It’s when your bone mass reduces, making bones fragile and break easily.1 Both women and men can get it, but it’s more common in women after menopause.1
Prevalence and Risk Factors
Osteoporosis affects people of all races, but white and Asian women are more at risk.1 Black and Hispanic women are also at risk.1 White men face more risk compared to African American and Mexican American men.1
Some risk factors include genetics, diet, hormones, and lifestyle.1 Knowing these can help find it early and manage it well.23
Causes of Osteoporosis
Osteoporosis happens when you lose too much bone mass and the structure of your bones changes. This may occur due to several risk factors. Elements like being female, getting older, and experiencing hormonal shifts are key. Also, things like what you eat and how you live can matter, such as not getting enough calcium and vitamin D, being inactive, or drinking and smoking too much. These aspects can put you at a higher risk for osteoporosis.
Age and Gender
Osteoporosis can affect anyone, but it’s more common as you age. Women usually have smaller and less dense bones than men, which puts them at a higher risk. Even though it’s less common, men over 70 are also vulnerable.1
Among women, those of white or Asian descent face higher risks. On the other hand, African American and Hispanic women have a lower chance, but it’s still a significant threat. For men, white non-Hispanics are at a higher risk than other groups.1
Hormonal Changes
After menopause, women’s estrogen levels drop, making osteoporosis more likely. Men can also suffer from osteoporosis, especially if their testosterone levels are low.1
In women, menopausal changes can quickly decrease bone density. Factors that increase this risk for women are early menopause, hysterectomy before age 45, and missed periods due to excessive exercise or dieting. Low testosterone levels in men can also raise their risk of osteoporosis.4
Dietary Factors
Not getting enough calcium and vitamin D in your diet can also lead to osteoporosis. People over 50 usually eat only half the recommended calcium. Plus, they often lack enough vitamin D.3
Lifestyle Factors
How you live matters too. Not being active, drinking a lot, and smoking can up your osteoporosis risk.14
Drinking alcohol heavily for a long time is especially bad for your bones. Smoking can also make you more likely to get osteoporosis and break your bones.1

Symptoms of Osteoporosis
Osteoporosis is often called a “silent” disease. This is because it usually shows no symptoms until a bone breaks.1 This condition makes bones so weak that they can break easily. This might happen after a small fall or when doing simple daily tasks like bending or coughing.1
Early Warning Signs
A stooped or hunched posture (kyphosis) can be one of the first signs of osteoporosis. It’s caused by fractures in the spine.1 These fractures can also bring a lot of back pain and make you lose height.1
Fracture Risk
The chance of getting a fracture with osteoporosis goes up a lot. Most of these fractures happen in falls. Out of these falls, 5% cause broken bones, 10% lead to a serious injury, and 30% result in any type of injury.3 Also,1 osteoporosis is the top reason for breaks in older women after menopause and in older men. The most common broken bones are the hip, backbone, and wrist.1 This is a major concern for the elderly.1
Diagnosis of Osteoporosis
Doctors diagnose osteoporosis with bone tests and imaging.5 By using bone mineral density (BMD) tests, they can predict breaks and check if treatments work.5 A common test, dual-energy x-ray absorptiometry (DXA), measures bone density. It’s vital for diagnosing osteoporosis.5
Bone Density Tests
For women over 65 or those with risks, doctors suggest osteoporosis tests.5 Not enough evidence exists for men’s screening.5
If a minor fall breaks your bone, you might need a bone density test.6 Treatment choices hinge on your 10-year bone break risk, from the test.6
Imaging Tests
X-rays and other imaging find bone loss and check break risk.5 Osteoporosis exams also look at posture, balance, muscle, and weight.5


These tests catch osteoporosis early, preventing breaks.5 Yet, screening’s benefit for men isn’t clear.7
Treatment Options for Osteoporosis
Treating osteoporosis needs a mix of methods. Meds are important, but so are lifestyle changes and taking the right supplements.6
Lifestyle Changes
Adding weight-bearing exercises can make a big difference if you have osteoporosis. Include walks, jogs, and dance in your routine. These activities help make your bones stronger and fight off the disease.6 Eating a balanced, calcium-filled diet is key. Don’t forget to quit smoking and cut down on alcohol. This also helps keep your bones healthy.6
Calcium and Vitamin D Supplements
Calcium and vitamin D are must-haves for strong bones. If your diet doesn’t give you enough, your doctor might suggest supplements.6
Medications for Osteoporosis
For those at high fracture risk, medications might be needed. These meds can slow bone loss or make bones denser. The most common are bisphosphonates, like Alendronate and Risedronate.68 If bisphosphonates don’t work for you, Denosumab could be an option.8 In tough cases, there are other meds that your doctor might consider, such as Teriparatide.68
A personalized plan is the best way to handle osteoporosis. It should include changes in how you live, along with the right supplements and meds. Follow what your doctor recommends to lower your fracture risk.689
Preventing Osteoporosis
Preventing osteoporosis is key to staying healthy. This bone disease can really affect your life10. Things like walking and dancing help make your bones stronger and prevent bone loss10. Eating foods with a lot of calcium and vitamin D is very important too10. Also, quitting smoking and not drinking too much can really help your bones10.
Exercise and Physical Activity
Doing exercises that put weight on your bones is great for preventing osteoporosis10. Many experts say it’s good to do these exercises 3 or 4 days a week10. Walking, jogging, dancing, and lifting weights can all help you build and keep strong bones.
Dietary Recommendations
Your diet plays a big role in your bone health10. For example, women who are older might need more calcium than younger women10. Vitamin D is also very important10. It’s good to eat enough protein too, about 0.4 grams for each pound you weigh10.
Quitting Smoking and Limiting Alcohol
Smoking and drinking too much can really hurt your bones10. It’s better to quit smoking and drink less to avoid osteoporosis10. These changes help your bones stay strong and lower your risk of breaking a bone because of osteoporosis.
Fall Prevention for Osteoporosis Patients
Falls are a big concern for people with osteoporosis. About one-third of those over 65 fall each year.11 People with osteoporosis often get injured from falls, leading to broken bones.11 But, by making homes safer and doing balance and strength exercises, the chance of falling decreases. And this can make a big difference for those with osteoporosis.
Home Safety Measures
It’s key to fix dangers at home and outside to stop falls for osteoporosis patients.11 Inside, items like loose wires and rugs can make you trip.11 Outside, things like wet floors and bad paths can be dangerous.11 Putting grab bars in bathrooms and using tools to reach are good ideas.11 So is wearing shoes with flat heels and good grips.11 And, having strong lights inside and out is crucial too.11
Balance and Strength Training
Add balance and strength activities to your exercise plan to cut down on falls if you have osteoporosis.12 Doing high-intensity exercises helps lower the chances of breaking a bone.12 It also boosts how strong your bones are in certain areas.12 Studies show that exercises like these can stop falls and fractures in people with osteoporosis.13 These workouts make your balance, muscle strength, and self-care better, keeping you safe from harmful falls.
Osteoporosis in Men
Osteoporosis is often thought of as a problem mainly for women. However, can equally be at risk. Men start with lesser bone strength and may lose bone over time. This can lead to osteoporosis and more breaks.14 Things like getting older, low testosterone, some drugs, and health issues can up the risk.
Even though men usually have more bone strength early on, they can face osteoporosis later in life. By the time men hit 65, they often get . Lately, more and more men are breaking bones because of weak bones. This is not good news, as men don’t always get checked and treated for osteoporosis after breaking a bone.14
It’s key to check the state of a man’s bones and how likely he is to get a break. Doctors look at a T-score less than -2.5 to see if there’s osteoporosis. There’s also a tool called FRAX to help figure out how likely a fracture is based on different factors.14 But, unlike with women, there isn’t enough proof yet that men should get bone checks every year as they get older.14
Some things could make men more prone to . These include ongoing health issues, certain meds, low sex hormone levels, unhealthy living, weak muscles, and being 70 or older.14 The way to help with is similar to women. It involves eating right, changing how you live, working out, preventing falls, and maybe taking meds.14 Doing things like exercise, eating food with lots of calcium and vitamin D, not drinking too much alcohol, and quitting smoking can also keep bones strong and lessen the risk of breaks.14
| Key Findings from Osteoporosis Research in Men |
|---|
| The Dubbo Osteoporosis Epidemiology Study in 2004 found out how often elderly men and women got hip and other bone breaks.15 |
| In 2005, a way to predict how likely people with a hip break were to die in the hospital or in the next year was made. This was first tested then.15 |
| The European Vertebral Osteoporosis Study in 1996 checked many European men and women. They looked at how much their spines were bending.15 |
| In Rochester, Minnesota, between 1985 and 1989, researchers saw how many people had their spine break.15 |
| In 2006, a study published in Osteoporos Int talked about how men’s bones can get weak.15 |
| In a 1998 study, they saw how fractures of the spine and back pain connect.15 |
| In 2004, the journal Calcif Tissue Int looked at how many men were dealing with osteoporosis and breaks.15 |
| In 2009, Horm Res looked at kids with a rare bone issue to learn more about it.15 |
| In 1995, J Clin Endocrinol Metab studied a rare condition related to male and female hormones to see how it causes bone problems.15 |
These stats give us a deeper view of osteoporosis in men. They show how often it happens, what makes it more likely, and the harm it can cause to different groups of people. This helps us understand and tackle osteoporosis better.
Juvenile Osteoporosis
[Juvenile osteoporosis] is rare in kids and teens, but it’s serious. It means low bone density and a bigger chance of breaking bones before you’re 2016. We don’t know everything about why it happens, but genes, health issues, or how you live might play a part17.
If a kid has [juvenile osteoporosis], we don’t know exactly how many are affected17. Sometimes, a cause isn’t found. This often shows up just before puberty. Healthy children suddenly have weaker bones then17. Some medicines that can make bones weaker are anticonvulsants, corticosteroids, and more17.
Not moving enough due to sickness, not enough calcium and vitamin D, and too much hard exercise can hurt bones17. To help, we fix what’s causing it, eat foods high in calcium, and stay active. Sometimes, medicine adults use for weak bones is needed too17.
If bone problems are from other health issues or drugs, we call it secondary osteoporosis18. Things like juvenile arthritis or diabetes can start this. So can some medicines18.
Taking a lot of corticosteroids, having it in the family, or not playing sports can up the risk18. Signs include past broken bones and pain in the back, hip, or foot. Sometimes, the spine might curve or the chest sink in18.
After a kid breaks a bone, doctors do tests to check for [juvenile osteoporosis]. Those tests are X-rays, bone strength tests, and blood tests to look at minerals18. Treating it involves dealing with the root problem. Plus, doing things to help bones, eating right, and maybe taking medicines18.
Not treating [juvenile osteoporosis] can lead to more broken bones, growth problems, and spine or rib issues18. Staying healthy with the right exercises and food can stop it sometimes18.
To keep kids’ bones strong, we need to watch them closely. This means movement therapy and preventing falls18. Parents should talk to doctors about stopping bone issues if their kid has a long-term illness or takes certain medicines18.
Sometimes, kids get a special type of osteoporosis without a known cause16. This kind can lead to back, hip, and foot pain, and even change how they look16.
Doctors suspect [juvenile osteoporosis] if a child breaks a bone16. They look at family history and do tests on the bones and blood. This checks for correct mineral levels16. Then, they choose the best way to treat it based on the child’s health and age16.
Some kids with idiopathic [juvenile osteoporosis] get better without special treatment. But making sure they don’t lose more bone during growth years is key16.
Pregnancy, Breastfeeding, and Bone Health
When a woman is pregnant or breastfeeding, her body needs more calcium. This is to help the baby grow and produce milk.19 Yet, sometimes, a mom’s bone density can drop a bit. This usually gets back to normal after the breastfeeding period.19 But, in some cases, this decrease is larger. It might lead to osteoporosis as she gets older.19 Eating foods high in calcium and vitamin D is good. So is doing exercises that have you bear weight. These steps help keep bones strong at this vital stage.19
There are a few things that could make bone density issues more likely during pregnancy. These include having a family history of osteoporosis, eating disorders, digestive issues, or bone diseases.19 There’s also something called pregnancy-and-lactation-associated osteoporosis (PLO). It’s rare but can be severe. It might make bones more likely to break, especially in the hip or spine.19
Talks suggest that breastfeeding could actually help bones stay strong for life.19 But, it can still take about a year after birth for a mom’s bone density to return to normal. This is especially true if she’s breastfeeding.19 Eating the right foods is key. Foods high in calcium, like dairy, dark greens, and chia seeds, are important for bone health. This is true during and after pregnancy.19
In the time leading up to menopause, hormone therapy can lower the risk of osteoporosis later.19 It’s crucial for women to work with their doctors. Together, they can come up with a plan to keep bones strong. This should cover the pregnancy, breastfeeding, and menopause periods.19
| Statistic | Reference |
|---|---|
| Lactation delays postpartum bone mineral accretion and temporarily alters its regional distribution in women. | 20 |
| Transient osteoporosis of the hip in pregnancy. | 20 |
| Idiopathic osteoporosis during pregnancy. | 20 |
| Calcium absorption is significantly higher in adolescents during pregnancy than in the early postpartum period. | 20 |
| Bone mineral density changes during lactation: maternal, dietary, and biochemical correlates. | 20 |
| Hormonal and dietary regulation of changes in bone density during lactation and after weaning in women. | 20 |
| Parity and bone mineral density in middle-aged women. | 20 |
| Pregnancy and lactation confer reversible bone loss in humans. | 20 |
| Factors underlying changes in bone mineral during postpartum amenorrhea and lactation. | 20 |
| Elevated parathyroid hormone-related peptide levels after human gestation: relationship to changes in bone and mineral metabolism. | 20 |
Managing Osteoporosis Fractures
If you have osteoporosis, you’re more likely to get fractures in the hip, spine, and wrist.9 Figuring out the risk of a fracture is key to managing your osteoporosis. It helps your doctor know how to treat you better.21
Fracture Risk Assessment
Doctors look at a few things to see if you might get a fracture because of osteoporosis. They consider your age, sex, how dense your bones are, if you’ve had fractures before, and any medical issues or habits that can make your bones weaker.21 They might also use tools like the FRAX® to guess how likely you are to have a major fracture in 10 years.
Treatment for Fractures
If you break a bone, what your doctor does to fix it depends on where and how bad the break is.9 You might need a cast to keep the bone from moving while it heals.9 Pain medicine and drugs that help heal bones might also be part of your treatment. If your fracture is serious, surgery could be needed. Surgeons can use pins, plates, or screws to put your bone back in place.
The main goal of treating a fracture is to heal the bone, get you moving again, and stop more breaks from happening.21 You might need physical therapy to get stronger and more mobile after your fracture heals.
Osteoporosis and Other Medical Conditions
Osteoporosis risk increases with age, influenced by gender and lifestyle choices. Additionally, other medical conditions and their treatments can play a part.1 Knowing how these aspects connect is key to fighting osteoporosis.
Medications and Osteoporosis
Some medicines spike osteoporosis risk. These include glucocorticoids, antiepileptics, and cancer drugs.1 Using these drugs for a long time might cause bone loss and more fractures.
Comorbidities and Osteoporosis
Some health conditions make osteoporosis likely.22 For example, hyperthyroidism, hyperparathyroidism, and celiac disease can harm bones.22 Others, like rheumatoid arthritis, type 1 diabetes, and asthma, raise the risk too. This is often due to corticosteroid use.22
People with health problems such as lupus face greater osteoporosis risk, especially before age 30.22 The use of corticosteroids for lupus and rheumatoid arthritis is a major factor.22
Understanding the link between osteoporosis and other illnesses is crucial. This knowledge lets healthcare workers tackle bone health more effectively. It helps to lower fracture risk in those with multiple health issues.
Living with Osteoporosis
Living with osteoporosis means changing some daily habits to keep bones strong and avoid fractures.23 It’s important to do exercises that put pressure on your bones, eat foods full of calcium and vitamin D, and make your home safer to prevent falls.
Lifestyle Adjustments
People with osteoporosis should choose a healthy, active life.23 Exercises like walking, jogging, or dancing help make bones stronger and slow bone loss.23 A diet packed with calcium and vitamin D is key for bone health.23 It’s also vital to stop smoking and cut back on alcohol to lower the chance of fractures.
Staying active is crucial for those with osteoporosis.23 Exercise makes bones stronger, improves balance, and cuts the risk of falls.23 Talk to your doctor for advice on safe and helpful exercises.
Support and Resources
Living with osteoporosis is tough, but there’s help out there.24 Specialists like rheumatologists and physical therapists can give tailored advice and treatments for osteoporosis.
Groups like the Bone Health and Osteoporosis Foundation and American Bone Health have many resources.24 They offer educational materials, support groups, and the latest news on osteoporosis to help those with the disease and their families.
When talking to your doctor, feel free to ask about treatment, managing pain, and how to avoid falls.24 Sharing your thoughts openly is key to getting the best care for osteoporosis.
Osteoporosis Research and Clinical Trials
Current osteoporosis research and clinical trials are key. They help us learn more and find better ways to treat this bone disease. Scientists look into many things, like how to stop, find, and deal with osteoporosis. They also work on why it happens and how to make treatments better.25
The National Institutes of Health (NIH) back many osteoporosis research projects. These efforts have led to big steps forward. For example, a study including over 10,000 women after menopause has contributed a lot. Another study focused on 6,000 older men to find out why osteoporosis happens in them.25
Scientists are studying how our genes affect our bone health. They use big studies to find out more. The NIH also helps fund tests on new osteoporosis treatments. And they check out how things in our environment can affect our bone health.25
Osteoporosis clinical trials are also very important. They help try out new treatments and learn more about the condition. Each year, thousands join these trials. Many more people, millions actually, benefit from these studies.26
All clinical trials follow strict rules to keep volunteers safe. In the U.S., a trial needs a special group to oversee it (IRB) if it involves drugs or devices that the FDA watches over. It’s important to protect the people who help in these studies.26
Getting involved in osteoporosis research and clinical trials is important. It lets you help improve osteoporosis care. You might also have a chance to try out new treatments before they are widely available. This work is vital for making better ways to prevent, find, and treat osteoporosis.
Conclusion
Osteoporosis is a serious bone disease that can change someone’s life.27 It is becoming more common, especially in countries like Turkey and Sweden. Studies show a link between drinking caffeine and a higher risk of bone fractures.27
Learning about the causes and signs of osteoporosis helps you protect your bones.28 This knowledge is crucial, especially for women and white women, who face a bigger risk of breaking bones as they get older.28
Scientists are working hard to find ways to prevent and treat osteoporosis.27 This ongoing effort gives hope to those with the disease.28 Keeping up with the latest information and working closely with doctors can make a big difference in dealing with osteoporosis.
FAQ
What is osteoporosis?
Who is at risk for developing osteoporosis?
What are the causes of osteoporosis?
What are the symptoms of osteoporosis?
How is osteoporosis diagnosed?
What are the treatment options for osteoporosis?
How can osteoporosis be prevented?
How can falls be prevented for osteoporosis patients?
Is osteoporosis a concern for men as well?
Can children and adolescents develop osteoporosis?
How does pregnancy and breastfeeding affect bone health?
How are osteoporosis fractures managed?
How does osteoporosis relate to other medical conditions?
What lifestyle adjustments are needed for living with osteoporosis?
What is the current state of osteoporosis research and clinical trials?
Source Links
- https://www.niams.nih.gov/health-topics/osteoporosis
- https://www.bonehealthandosteoporosis.org/patients/what-is-osteoporosis/
- https://www.mayoclinic.org/diseases-conditions/osteoporosis/symptoms-causes/syc-20351968
- https://www.nhs.uk/conditions/osteoporosis/causes/
- https://www.niams.nih.gov/health-topics/osteoporosis/diagnosis-treatment-and-steps-to-take
- https://www.mayoclinic.org/diseases-conditions/osteoporosis/diagnosis-treatment/drc-20351974
- https://www.aafp.org/pubs/afp/issues/2015/0815/p261.html
- https://www.mayoclinic.org/diseases-conditions/osteoporosis/in-depth/osteoporosis-treatment/art-20046869
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5768298/
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/osteoporosis/what-you-can-do-now-to-prevent-osteoporosis
- https://www.bonehealthandosteoporosis.org/patients/treatment/exercisesafe-movement/preventing-falls/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1114702/
- https://www.osteoporosis.foundation/health-professionals/fragility-fractures/falls-prevention
- https://www.niams.nih.gov/health-topics/osteoporosis-men
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3557324/
- https://www.chop.edu/conditions-diseases/juvenile-osteoporosis
- https://www.niams.nih.gov/health-topics/juvenile-osteoporosis
- https://www.stanfordchildrens.org/en/topic/default?id=juvenile-osteoporosis-90-P01965
- https://www.hss.edu/article_pregnancy-bone-density.asp
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4266784/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9242734/
- https://www.webmd.com/osteoporosis/features/medical-causes
- https://www.nhs.uk/conditions/osteoporosis/living-with/
- https://www.medicalnewstoday.com/articles/living-with-osteoporosis
- https://www.niams.nih.gov/health-topics/osteoporosis/more-info
- https://www.bonehealthandosteoporosis.org/patients/clinical-trials/about-clinical-trials/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5335887/
- https://medicine.yale.edu/news-article/draw-an-informed-conclusion-preventing-osteoporosis/